15 Must-Know EKG/ECG Rhythms Every Nurse Should Master
Essential cardiac rhythms for nursing professionals: identification, clinical significance, and key nursing interventions for electrocardiogram (EKG/ECG) interpretation
Disclosure: This post contains affiliate links. As an Amazon Associate, we earn from qualifying purchases at no extra cost to you.
🚀 Practice with Our Interactive EKG/ECG Simulator
Want to practice identifying these rhythms? Try our free EKG simulator with real-time rhythm generation and quiz mode!
Start Practicing NowWhy EKG/ECG Rhythm Recognition Matters
As a nursing professional, your ability to quickly and accurately identify EKG (electrocardiogram) rhythms—also known as ECG rhythms can be the difference between life and death. Whether you're working in the ICU, emergency department, medical-surgical unit, or any cardiac monitoring environment, these 15 essential rhythms form the foundation of cardiac care knowledge.
This comprehensive guide covers the most critical EKG/ECG rhythms every nurse encounters, providing you with the key features, clinical significance, and nursing considerations for each. Master these rhythms to enhance your clinical confidence and improve patient outcomes.
The Essential 15: Must-Know EKG/ECG Rhythms
Normal Sinus Rhythm (NSR)

Key Features:
- P wave before every QRS complex
- Consistent PR intervals
- Regular R-R intervals
- QRS width < 0.12 seconds
Clinical Significance
Normal cardiac rhythm indicating proper SA node function and conduction system integrity.
Sinus Bradycardia
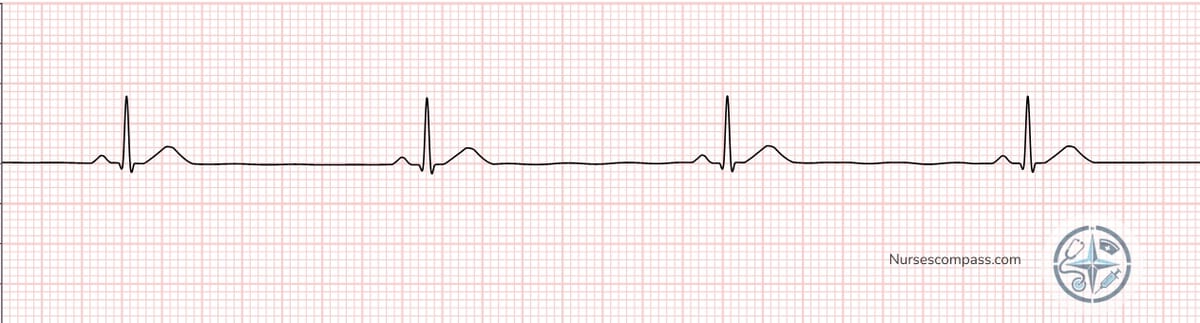
Key Features:
- All NSR features but rate < 60 bpm
- May be physiologic in athletes
- Can indicate increased vagal tone
Nursing Considerations
Monitor for symptoms of decreased cardiac output: dizziness, fatigue, chest pain, or syncope. Consider causes like medications, hypothermia, or increased intracranial pressure.
Sinus Tachycardia
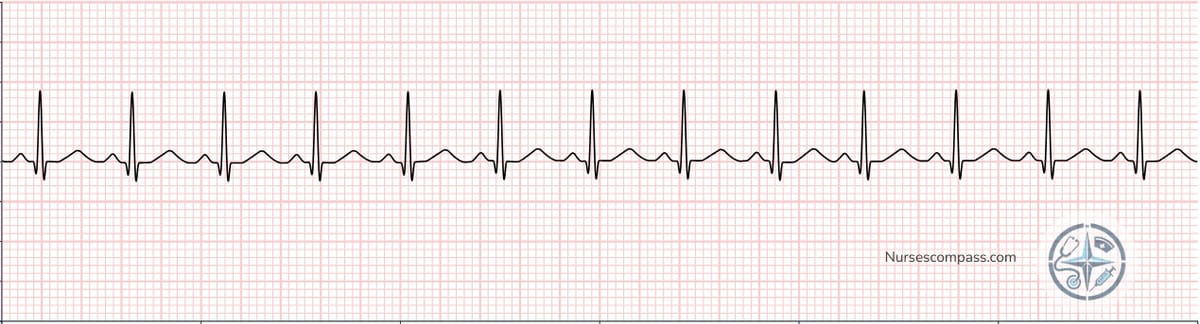
Key Features:
- All NSR features but rate > 100 bpm
- P waves may be difficult to see
- Usually compensatory response
Nursing Considerations
Identify and treat underlying causes: fever, pain, anxiety, hypovolemia, hypoxia, or medications. Monitor for signs of decreased cardiac output at very high rates.
Atrial Fibrillation (AFib)

Key Features:
- No discernible P waves
- Undulating baseline (fibrillatory waves)
- Irregular R-R intervals
- QRS usually narrow
Clinical Significance
High stroke risk due to atrial stasis and clot formation. May cause decreased cardiac output and heart failure exacerbation.
Nursing Considerations
Monitor for stroke symptoms, assess for anticoagulation therapy, evaluate hemodynamic stability. Document pulse deficit if present.
Atrial Flutter

Key Features:
- Classic sawtooth flutter waves
- Regular or irregular ventricular response
- No true P waves
- Common 2:1 conduction ratio
Nursing Considerations
Monitor for hemodynamic compromise with rapid ventricular response. Prepare for cardioversion if unstable. Assess for embolic risk.
Supraventricular Tachycardia (SVT)
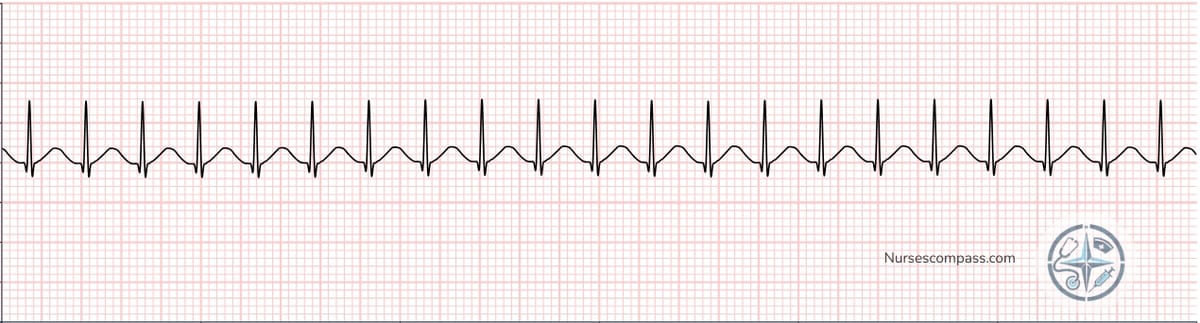
Key Features:
- Very regular, rapid rhythm
- Narrow QRS complexes
- P waves often not visible
- Abrupt onset and termination
Nursing Considerations
Try vagal maneuvers if stable. Prepare adenosine for IV administration. Monitor for hemodynamic compromise and chest pain.
Ventricular Tachycardia (VT)
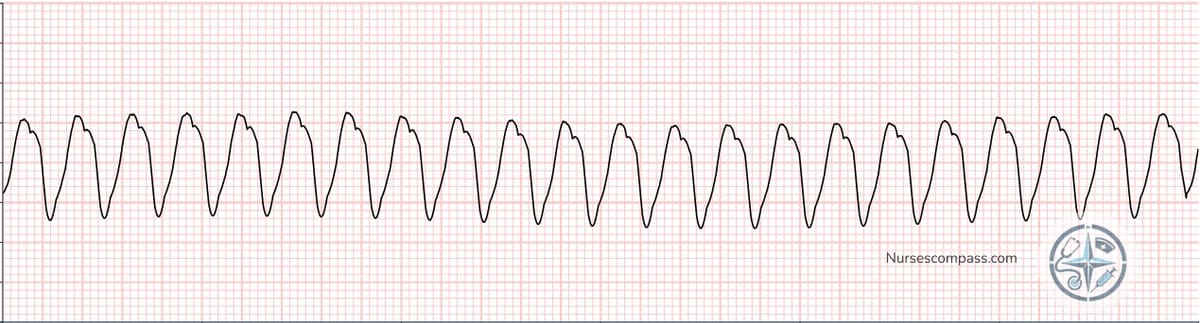
Key Features:
- Wide, bizarre QRS complexes
- Regular rapid rhythm
- AV dissociation may be present
- Potentially life-threatening
Clinical Significance
Life-threatening rhythm that can degenerate into ventricular fibrillation. Immediate intervention required if patient is unstable.
Nursing Considerations
Assess pulse and consciousness immediately. If unstable, prepare for cardioversion. If stable, prepare antiarrhythmic medications. Have crash cart ready.
Ventricular Fibrillation (VF)
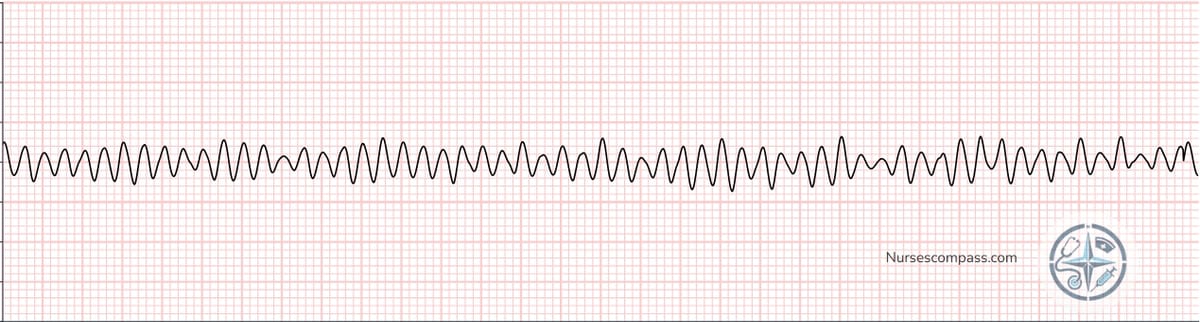
Key Features:
- Chaotic, wavy baseline
- No identifiable complexes
- Amplitude may vary
- Fatal without immediate intervention
Clinical Significance
Cardiac arrest rhythm. No cardiac output. Death within minutes without immediate defibrillation and CPR.
Nursing Considerations
IMMEDIATE defibrillation required. Begin high-quality CPR. Follow ACLS protocol. This is a medical emergency.
⚡ Master EKG Rhythms with Essential Reference Cards
30 Horizontal Nursing Badge Reference Cards
Complete EKG rhythm reference, lab values, and vital signs - everything you need for confident clinical practice.
Asystole
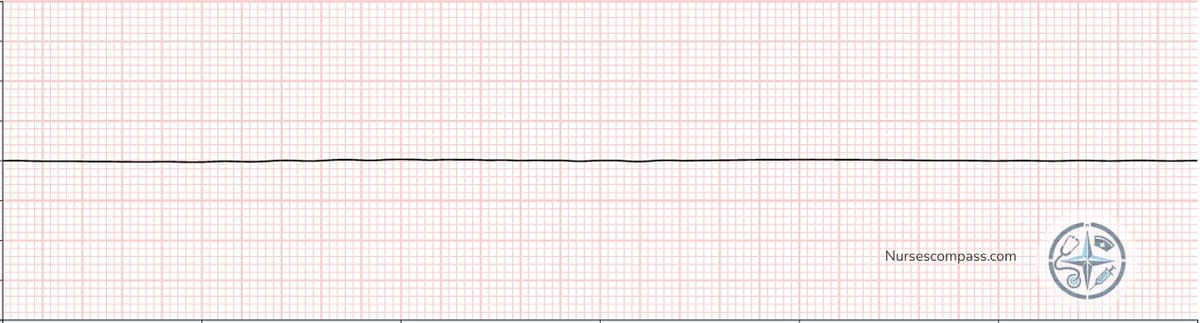
Key Features:
- Flat line (no electrical activity)
- Confirm in multiple leads
- Check all connections
- Worst possible rhythm
Nursing Considerations
Confirm true asystole in multiple leads. Begin high-quality CPR immediately. Follow ACLS protocol. Consider reversible causes (H's and T's).
First-Degree AV Block
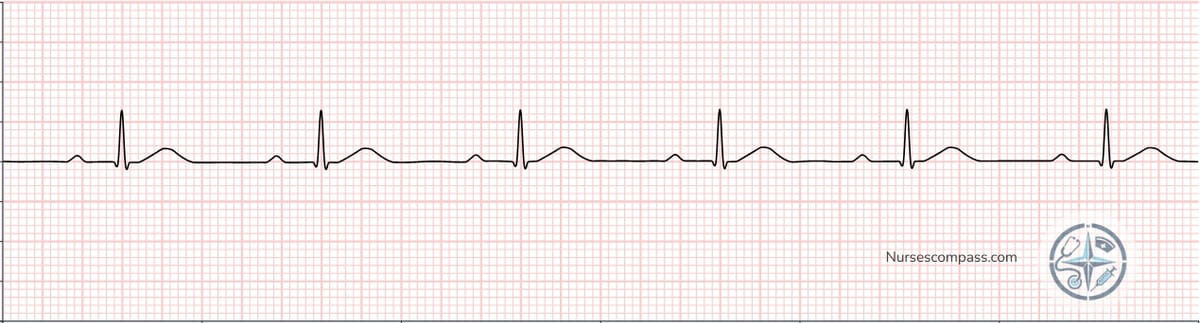
Key Features:
- Prolonged but consistent PR intervals
- Every P wave followed by QRS
- Often benign finding
- May be medication-related
Nursing Considerations
Usually benign but monitor for progression to higher-degree blocks. Review medications (digoxin, beta-blockers, calcium channel blockers).
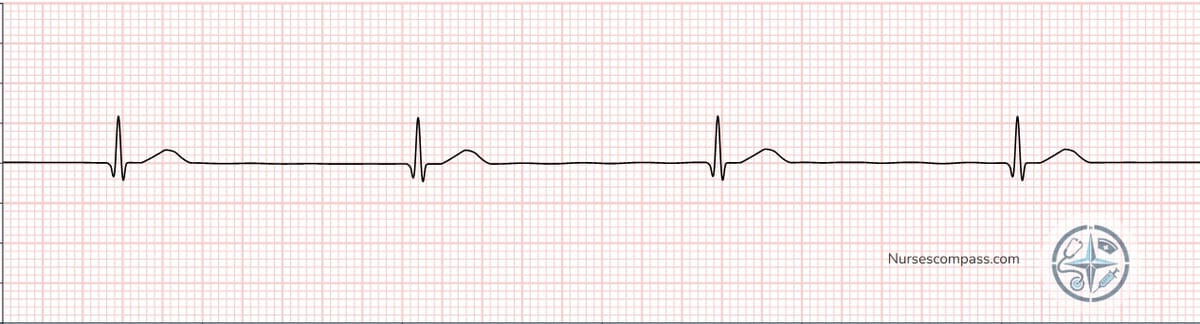
Complete Heart Block (3rd Degree)

Key Features:
- P waves and QRS complexes independent
- Regular P-P and R-R intervals
- More P waves than QRS complexes
- Escape rhythm provides QRS
Clinical Significance
Serious conduction disturbance requiring immediate intervention. High risk for cardiac arrest and hemodynamic compromise.
Nursing Considerations
Monitor closely for symptoms of decreased cardiac output. Prepare for temporary pacing. Consider permanent pacemaker placement.
Premature Ventricular Contractions (PVCs)

Key Features:
- Early, wide QRS complexes
- No preceding P wave
- Compensatory pause usually follows
- May be unifocal or multifocal
Nursing Considerations
Count frequency and assess patterns. Monitor for runs of VT. Frequent PVCs may indicate electrolyte imbalance or cardiac ischemia.
Junctional Rhythm
Key Features:
- No P waves or inverted P waves
- Regular, narrow QRS complexes
- Escape rhythm from AV junction
- Rate typically 40-60 bpm
Nursing Considerations
Monitor for symptoms of bradycardia. May indicate SA node dysfunction or increased vagal tone. Assess underlying cause.
Premature Atrial Contractions (PACs)

Key Features:
- Early P waves with different shape
- Usually followed by narrow QRS
- May have noncompensatory pause
- Often benign finding
Nursing Considerations
Usually benign but frequent PACs may trigger atrial fibrillation. Monitor pattern and frequency. Assess for caffeine intake or stress.
Pulseless Electrical Activity (PEA)
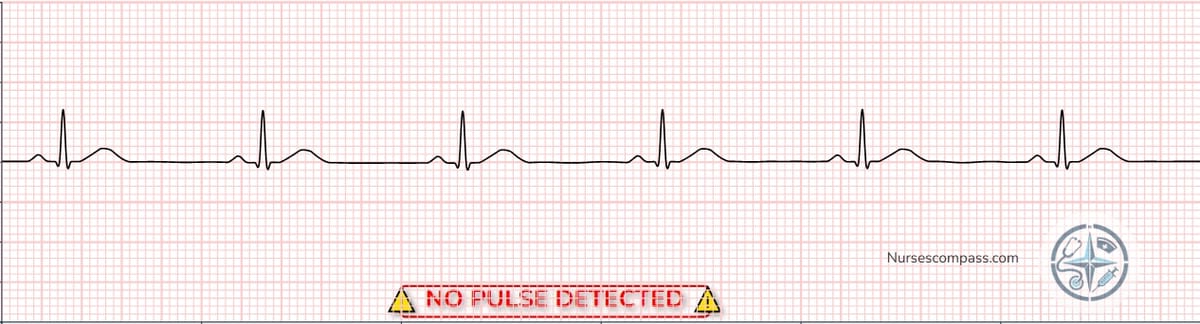
Key Features:
- Organized electrical activity on monitor
- No palpable pulse
- Patient in cardiac arrest
- Requires immediate CPR
Clinical Significance
Cardiac arrest rhythm. Despite electrical activity, there is no effective cardiac output. Often due to reversible causes.
Nursing Considerations
Begin high-quality CPR immediately. Follow ACLS protocol. Aggressively search for and treat reversible causes (H's and T's).
🎯 Key Takeaways for Nursing Practice
Mastering these 15 essential EKG rhythms provides the foundation for safe cardiac care. Remember that rhythm recognition is just the first step – always correlate your findings with the patient's clinical presentation and hemodynamic status.
Quick Assessment Framework:
Rate → Rhythm → P waves → PR interval → QRS width → Clinical correlation
📚 Continue Your Learning
❓ Frequently Asked Questions
🚀 Ready to Practice?
Test your knowledge with our free EKG simulator featuring all these rhythms and more!
Practice EKG Rhythms Now📚 Essential Study Resources for Nursing Success
Master EKG interpretation and critical nursing skills with these comprehensive study guides.
EKG | ECG Interpretation Made Easy
Step-by-step ECG strip interpretation with detailed examples and practice strips.
Looking for more nursing tools and resources?
🛍️ Browse All Nursing Essentials⚠️ Medical Disclaimer
This content is for educational purposes only and is NOT intended for clinical use, patient care, or emergency situations. Always consult current medical protocols, facility guidelines, and healthcare providers for patient care decisions. Do not use this information for patient diagnosis or treatment.
📚 References & Sources ▼
Click to view 3 sources cited
